January 14th, 2024
Written by: Margaret Gardner
First, I need you to promise not to panic. What I’m about to tell you sounds pretty, well… freaky. You promise? Good.
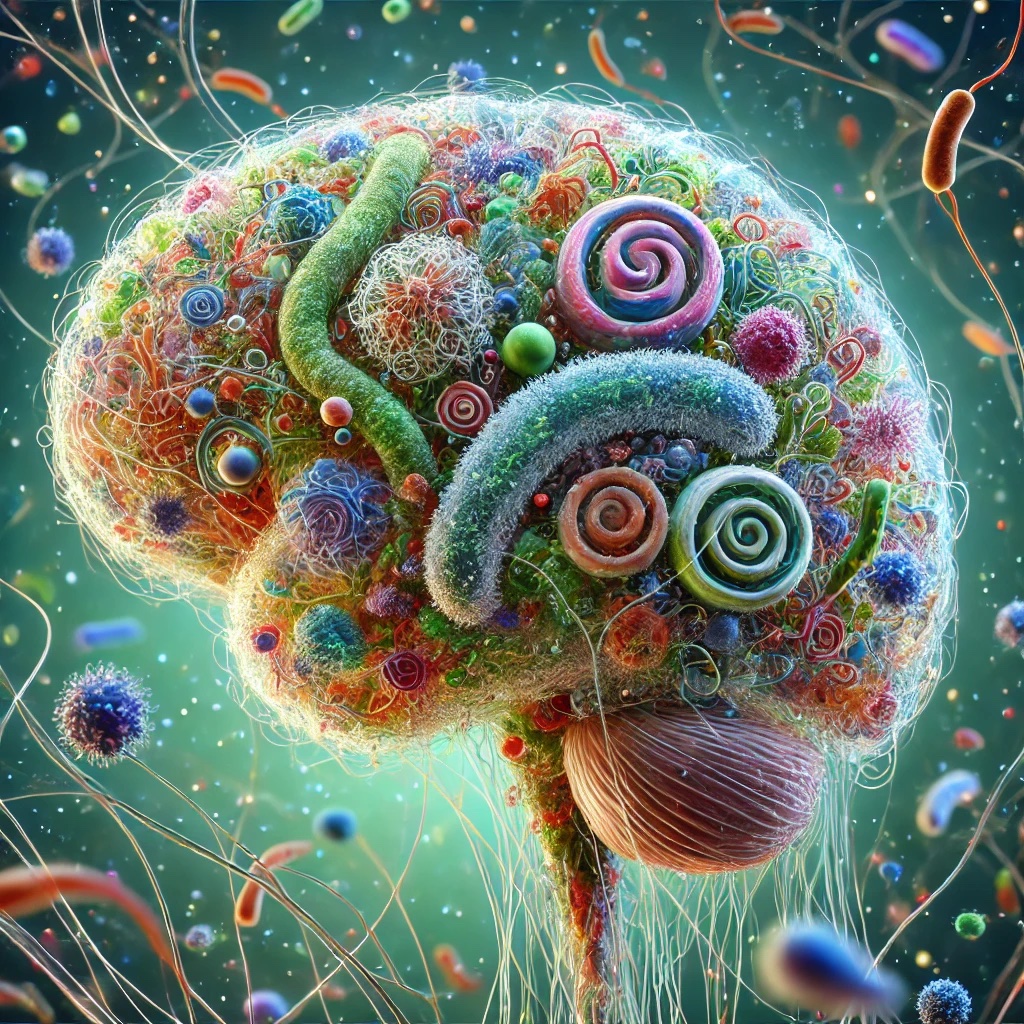
There might be bacteria and fungi living in your brain. And my brain. Maybe all of our brains. We don’t know for sure. But although it sounds like the plot to a Black Mirror episode, the existence of a brain microbiome is one of the hottest new controversies in neuroscience. While we know that the human body holds millions of microbes – or microorganisms like bacteria, fungi, and viruses1 – their presence in the brain is uncertain. Together, we’ll look at the evidence for and against the existence of these tiny inhabitants and their possible role in neurological disease.
In Health?
The word “microbiome” refers to all the bacteria, fungi, and viruses that live in and on different parts of our bodies2. If you’ve heard about the microbiome before, it’s probably because of the gut microbiome that lives in our digestive system and helps us break down food. While it was once a controversial idea, scientists now know that these microbes influence (and are influenced by) the brain. Changes in gut bacteria have even been linked to mood disorders like depression (see this PNK article for a great overview). But what if there are other microbes affecting the brain – and in this case, the call is coming from inside the house?
A research group in Canada were studying brain injury from HIV, where the virus’s infiltration of immune cells triggers them to damage other cells in the brain. Hypothesizing that this injury was caused by microbes, they compared microbes in the brain tissue of deceased individuals with HIV to healthy brain samples. The big surprise came when they found that the microbe profiles of both groups were incredibly similar, with one class of bacteria in every sample tested3. This suggests that, rather than being a fluke of a particular person or how the samples were tested, it means this group of bacteria really are in all our brains. To further prove this point, they tested samples from monkeys, who are closely related to humans, and found the same class of bacteria in their brains, too3. Finally, they even found that transplanting small pieces of human brain tissue into mice caused their brains to house the same types of bacteria3. This shows that 1) the bacteria really were there in the human brain sample and 2) because the mice did not get sick after getting the bacteria, these microbes can just hang out in healthy brains without causing problems3,4.
So, there we have it, our brains are full of microbes, right? Well, not quite. There are many reasons why tests for bacteria in brain tissue could come back positive, even if there isn’t any in the brain. First, there’s the possibility of contamination: bacteria are around us all the time, and it’s likely that some live in the chemicals and equipment used to collect and test brain tissue samples4. Second, scientists have recently come to agree that human blood has a microbiome of its own. This means that, although microbes might flow through the brain via the bloodstream, they might remain confined to blood vessels and never exit into the brain tissue itself – until a scientist cuts through the brain tissue to take a sample4. Finally, researchers often look for microbes by testing for snippets of their DNA. However, it’s possible that the tissue samples just have so much human DNA – some of which looks a little bit like bacteria DNA – that tests mistakenly flag human DNA as a microbe5. Any number of these explanations might account for why some studies find bacteria in healthy brain tissue while others do not4,5.
In Sickness?
Scientists have known for a long time that certain disease-causing microbes – such as COVID-19, Zika virus, Streptococcus bacteria, and HIV – can harm the brain, either by sneaking past its defenses or as a side effect of damage elsewhere in the body5. In recent years there has been a renewed interest in researching how microbes might cause neurodegenerative diseases, which cause the brain’s functions to breaks down over time. People with neurodegenerative diseases also tend to have lots of inflammation, or immune system activity that’s so intense it can cause collateral damage to the body (or in this case, brain tissue). Picture a battle where the Immune Army is trying to defend its homeland from invaders, but the battle is so long and intense that both sides end up harming of the landscape around them. Researchers are now theorizing that some neurodegenerative diseases are due to a microscopic battle between the immune system and microbes, with damage caused by either or both sides leading to the disease’s sympoms5.
The most direct way of trying to link microbes with neurodegenerative disease is to take samples of human brain tissue from individuals with a neurodegenerative disease and check if there are microbes, how many there are, and what kinds. Most research of this kind has focused on Alzheimer’s disease, with many studies finding high levels of bacteria and fungi in patients’ brains5. A smaller body of evidence suggests that microbes could cause and/or contribute to several neurodegenerative disorders, like amyotrophic lateral sclerosis (ALS), Parkinson’s disease, and Huntington’s disease5. One particularly interesting study used brain tissue taken from living individuals with multiple sclerosis (MS), who sometimes have brain samples taken as part of diagnosis, and those with epilepsy, who sometimes have brain samples removed as part of treatment. Besides finding far more microbes in the MS group overall, the authors found that one MS patient, who had two biopsies a few months apart, went from having about the same number of bacteria as the control samples to having several different microbes as their condition progressed5,6. This could mean that the increase in bacteria caused their symptoms to worsen over time. (Side note: The first author of this study has a pretty cool blog that goes into greater detail on this work, if you’re looking for a nerdy internet rabbit hole).
Unfortunately, the picture is not so cut and dry. Almost as many studies have failed to find evidence of elevated microbes in neurodegenerative brain tissue, and those that do often find a variety of different kinds of microbes across individuals5. Scientists also don’t know if the microbes cause a given neurodegenerative disease, or if the disease has weakened the brain’s defenses, allowing microbes to creep in. In other words, they can’t tell if the microbes are a cause or a symptom of a given neurodegenerative disease. Overall, while more research is needed to link specific microbes with specific neurodegenerative diseases (or disease subtypes), the idea that microbes could cause or worsen neurological symptoms is much less controversial among researchers than the possibility of a microbiome being part of a healthy human brain.
So, are there microbes in our brains? Are they bad for us? We’ll need a lot more research to say whether there is a brain microbiome, for better or for worse. But with more and more neuroscientists looking, we may be on the edge of an incredible scientific breakthrough – or just passing a bump in the road.
References
1. In brief: What are microbes? In: InformedHealth.Org [Internet]. Institute for Quality and Efficiency in Health Care (IQWiG); 2022. Accessed January 6, 2025. https://www.ncbi.nlm.nih.gov/books/NBK279387/
2. Microbiome. National Institute of Environmental Health Sciences. Accessed January 6, 2025. https://www.niehs.nih.gov/health/topics/science/microbiome
3. Branton WG, Ellestad KK, Maingat F, et al. Brain Microbial Populations in HIV/AIDS: α-Proteobacteria Predominate Independent of Host Immune Status. PLOS ONE. 2013;8(1):e54673. doi:10.1371/journal.pone.0054673
4. Link CD. Is There a Brain Microbiome? Neurosci Insights. 2021;16:26331055211018709. doi:10.1177/26331055211018709
5. Arabi TZ, Alabdulqader AA, Sabbah BN, Ouban A. Brain-inhabiting bacteria and neurodegenerative diseases: the “brain microbiome” theory. Front Aging Neurosci. 2023;15. doi:10.3389/fnagi.2023.1240945
6. Kriesel JD, Bhetariya P, Wang ZM, Renner D, Palmer C, Fischer KF. Spectrum of Microbial Sequences and a Bacterial Cell Wall Antigen in Primary Demyelination Brain Specimens Obtained from Living Patients. Sci Rep. 2019;9(1):1387. doi:10.1038/s41598-018-38198-8
Leave a comment