February 5, 2019
Written by: Carolyn Keating
It’s a popular television troupe: an important character falls into a coma. Maybe the coma occurs right after the character resolves some important personal issue, or maybe it allows the character to have a dream that reveals important details about the plot. Sometimes the comatose person responds to their loved ones voices or touch. TV shows usually portray these characters having miraculous, speedy recoveries; rarely does the person remain in a vegetative state or not survive. But just how accurate are these depictions? What exactly is a coma, and how is it different from conditions like vegetative state?
Coma is just one of several disorders of consciousness, which occur when the state of being awake and aware of your surroundings is impaired. Wakefulness and awareness are the two main components of consciousness. When you are awake (also called aroused or vigilant), sensory information from the environment can be detected by the brain. Awareness requires a little more brain power; it occurs when this incoming sensory information can be processed, so that you’re aware of the environment and yourself. For example, someone who is awake will be able to open their eyes, but someone who is also aware will be able to move their eyes, including in response to a command. The degree of wakefulness and awareness a person displays determines their level of consciousness. But before we can discuss the various disorders of consciousness and how the brain is involved, we first have to understand how the brain produces wakefulness and awareness to begin with.
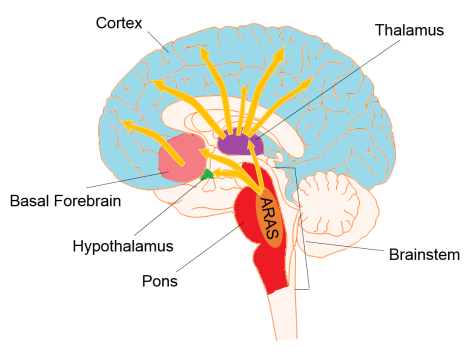
Distinguishing circuits that are only involved in wakefulness or awareness can be difficult since the two states are intertwined. For instance, can you imagine being aware of something without being awake? Further complicating the problem is that some structures thought to be important for one state are highly interconnected to structures involved with the other state. Nevertheless, scientists have identified regions that are necessary for one state or the other (Figure 1). In general, the cerebral cortex is important for things like thought, attention, and language, while structures beneath the cortex are responsible for our more basic survival needs. As such, wakefulness depends on a network of cells in the brainstem termed the ascending reticular activating system, or ARAS. In particular, neurons from a structure called the pons communicate with areas called the thalamus, hypothalamus, and basal forebrain. These connecting structures then send arousal signals up to the cortex. Awareness, on the other hand, depends on intact connections within the cortex itself, as well as between ARAS and the cortex, especially with the thalamus1. Now that we know which brain circuits are involved in wakefulness and awareness, let’s take a closer look at these disorders of consciousness and what happens in the brain to produce them.
Coma
In coma, much like during sleep or anesthesia, a person is neither awake nor aware. They lie with their eyes closed and are not conscious of themselves or their surroundings. Unlike people who are sleeping, patients in comas cannot be woken up with sound, shaking, pain, or any other environmental stimuli. This period of unconsciousness is usually prolonged, but normally patients gradually begin to awaken and recover in 2-4 weeks2.
A coma is a medical emergency, and indicates that there are some serious problems going on in the brain. Comas are usually caused by traumatic head injury, stroke, or drug/alcohol intoxication. A person in a coma typically has damage to regions vital to wakefulness, such as the ARAS in the pons division of the brainstem. Patients could also have damage in the thalamus and to axons throughout the cortex, which makes it hard for neurons to communicate with each other in these parts of the brain crucial for awareness1,2.
Though many comas are the result of the medical emergencies described earlier, in some extreme cases they are actually induced intentionally. These medically-induced comas are used by doctors to protect the brain during major neurosurgery or to alleviate brain swelling after a traumatic injury3. These temporary deep states of unconsciousness are produced by administering barbiturates, central nervous system depressants like pentobarbital or propofol4. Barbiturates protect the brain after traumatic injury by reducing the brain’s metabolism and blood flow. Importantly, doctors can control when a patient emerges from the induced coma and regains consciousness by removing the barbiturates.
Vegetative State
As a person emerges from a coma, they pass through other states of altered consciousness before returning to “normal”. One of these conditions is vegetative state (also known as Unresponsive Wakefulness Syndrome), when patients are awake but not aware of themselves or their environment. Their body functions, but they aren’t processing any sensory information or having any thoughts2. Someone in a vegetative state can improve over weeks or years, and in fact spontaneous recovery has been observed 5-10 years after injury1.
It has been hard for scientists to study emergence from coma, but they have some ideas about what might be going on in the brain to produce altered consciousness. Damage to the ARAS, basal forebrain, or thalamus can produce an unaware state but still produce enough activation to achieve wakefulness, especially if there is minimal damage to hypothalamus. Interestingly, evidence seems to suggest that damage to the cortex isn’t required to produce wakefulness without awareness. But further study is needed to confirm exactly which brain regions are essential for producing these states of altered consciousness1.
Minimally Conscious State
The category of minimally conscious state is for patients who are not in a vegetative state, but are still not able to communicate consistently. They show evidence that they are aware of themselves or their environment, but not all the time or not to the extent that a “normal” person would. For instance, they could indicate yes or no in response to a question (although their answer might not be accurate), or make purposeful movements (more than a simple reflex) in response to something in their environment2.
In the brain, what seems to differentiate people in a vegetative state from those in a minimally conscious state is activity in two regions: the medial parietal cortex (or precuneus) and the adjacent posterior cingulate cortex. These areas are among the most active brain areas in people who are conscious and awake, and the least active in people who are sleeping or anesthetized2. While scientists still aren’t sure exactly what happens as a patient emerges from unconsciousness, it’s possible that they pass through these different states as more arousal information is able to reach the cortex, where a person can become aware of it.
Is there anything doctors can do help someone recover from a disorder of consciousness? Some experimental therapies use electricity to try to increase the brain activity in certain regions that are improperly diminished. Other treatments involve administering drugs that are thought to indirectly activate the thalamus, one region connecting the brainstem to the cortex1. Hindering progress, however, is the fact that diagnosing disorders of consciousness can be difficult, as the tests that doctors perform usually assume that the person has an intact nervous system outside of the brain (which is not always the case). New advances in brain imaging and EEG technology to directly measure brain responses that would produce movement or speech if the peripheral nervous system were healthy have detected cases of “covert awareness” that otherwise would have gone unnoticed2. Going forward, further understanding different disorders of consciousness should help doctors make correct diagnoses and develop new treatments.
References
- O’Donnell, J. C. et al. Challenges and Demand for Modeling Disorders of Consciousness following Traumatic Brain Injury. Neurosci. Biobehav. Rev. 0–1 (2018). doi:10.1016/j.neubiorev.2018.12.015
- Laureys, S., Owen, A. M. & Schiff, N. D. Brain function in coma, vegetative state, and related disorders. Lancet Neurol. 3, 537–546 (2004).
- The Brain Trauma Foundation. The American Association of Neurological Surgeons. The Joint Section on Neurotrauma and Critical Care. Use of barbiturates in the control of intracranial hypertension. J. Neurotrauma 17, 527–530 (2000).
- Brown, E. N., Lydic, R. & Schiff, N. D. General anesthesia, sleep, and coma. N. Engl. J. Med. 363, 2638–2650 (2010).
Images
Figure 1 adapted from Motifolio Neuroscience Illustration Toolkit.
