November 26th, 2024
Written by: Julia Riley
Mental health disorders are a common and often stigmatized affliction in today’s society. Over 1 in every 5 adults in the United States are coping with the symptoms of at least one mental health disorder1. Despite how common mental health issues are, their treatment is far from straightforward compared to other illnesses. When someone goes to the doctor with an infection, the doctor will consider the infection itself, the patient’s medical history, and the course of treatment the patient is most likely to follow before prescribing the appropriate treatment. Like any other illness, the treatment for an individual’s mental illness must be specifically informed by their symptoms, their individual biology, and their medical history. However, the brain is an unique organ with nuanced differences from person to person, and it’s difficult to understand what’s going awry in mental illness; this is especially true in that doctors cannot easily run foolproof diagnostic tests for different mental health issues due to our insufficient understanding of how different mental illnesses are specifically reflected in the body’s chemistry and the brain’s activity. A better understanding of how our treatments for mental illnesses impact the brain is necessary in order to more effectively help the people affected.
A relatively modern class of treatments for mental health disorders uses methods that directly alter brain activity in order to give patients relief from their symptoms. Here, we will discuss a relatively modern treatment for depression called TMS that uses powerful magnets to directly alter brain activity, unpack how it is improving our understanding of mental health, and explore why it holds promise as a treatment for other mental illnesses. Importantly, the fact that directly altering the brain’s activity provides relief from such symptoms directly contradicts the antiquated belief that these disorders result from lack of willpower or character flaws. Instead , these developments support the concept that mental health disorders should be treated as the result of physical, underlying abnormalities that are not necessarily in the patient’s full control.
Neuromodulation: What it is and why it’s used
One of the most common and effective means of combatting mental illness is talk therapy2,3. However, therapy is not always sufficient, and its effectiveness varies depending on many factors that include the illness and person in question. This is because each person has a unique combination of biology, socioeconomic status, childhood experiences, and other aspects of their identity that help shape how their brain functions. Thus, it is sometimes necessary to simultaneously treat mental health issues via clinical interventions such as medication. Psychiatric medication is a common next step for clinical intervention when talk therapy is not sufficient to help patients cope with their symptoms, and is effective for many people4. However, psychiatric medications have their drawbacks just like any medications do, and there are cases where they are not effective enough to sufficiently improve a patient’s quality of life4.
When these approaches fail, there is another class of modern treatments called neuromodulation that alters the brain even more directly than other forms of clinical intervention5. This approach is typically reserved for patients who continue to struggle with mental illness after trying therapy and medication; this is likely because it requires specialized equipment that is not found at every medical facility, trained staff to administer treatments, and usually needs to be administered over numerous sessions in order to be effective, making it relatively difficult to access compared to other clinical interventions for mental illness. Neuromodulation is the practice of applying external sources of energy such as magnets or electricity to the brain5,6. Because brain cells communicate with each other using electricity, introducing external sources of energy can alter your brain activity, effectively “rewiring” the way your brain functions7. This is a powerful approach for several reasons. The first is that your brain is built to continuously strengthen and rely on the connections it uses the most frequently8. In many situations, this is a good thing; it means that the more times you do something, the more easily you can do it the next time. A good example is that someone who has been playing a sport for ten years might be more likely to quickly and accurately predict the other team’s next move than someone who has been playing for one year. However, in the context of a mental illness like depression whose symptoms can include loss of pleasure, feelings of worthlessness, and withdrawing from others, this also means that people who have been depressed for a prolonged period of time could have brains that default to using the brain pathways underlying their depressive thought patterns regardless of whether it is appropriate for the situation. In our sports analogy, this would be like a soccer player trying out street hockey and instinctively trying to kick the puck instead of using their stick to hit it toward the goal. By using neuromodulation techniques, doctors can interfere with the brain’s set pathways, strengthening healthy pathways and steering the brain away from harmful ones. This is thought to allow the patient a cleaner slate with which they can start to strengthen alternative brain pathways and develop healthier patterns of thinking.
Transcranial Magnetic Stimulation (TMS) as a neuromodulatory approach to treat mental illness
Although effective in many cases, neuromodulatory approaches are relatively new compared to most psychiatric therapies. Several groups of scientists are hard at work trying to understand how neuromodulation works, who is most likely to benefit from it, and what the long-term consequences and side effects might be with regards to patient’s abilities to think, feel, and function. One specific type of neuromodulation is called transcranial magnetic stimulation (trans for across, cranial for head or skull; hereafter referred to as TMS; Figure 1).
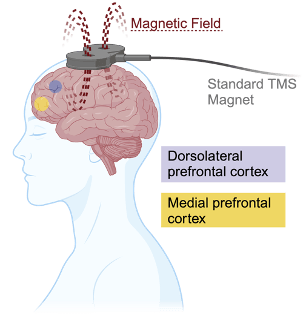
With TMS, special magnets are used to send waves of energy through the skull and into a specific area in the brain5,7. Because magnetic fields are able to stimulate electrical activity between brain cells, clinicians can use TMS to silence or activate the cells in a variety of brain areas, allowing them to temporarily change that brain area’s overall level of activity7. Since different tasks require different brain areas and different mental illnesses can impact different brain areas, this increases the potential versatility of TMS as a clinical tool for the treatment of mental health disorders. TMS also has the benefit of not having the side effects of many psychiatric medications and has been safely employed millions of times in clinical settings.
TMS as a treatment for depression
In 2008, the United States Food and Drug Administration approved the clinical use of TMS for patients with medication-resistant depression9. Typically, these patients receive several rounds of TMS specifically targeting an area of the brain called the dorsolateral prefrontal cortex, which sits near the front of your head on the top left side (Figure 1)7. The dorsolateral prefrontal cortex acts like a busy intersection important for many thought-intensive tasks, including the ability to weigh emotional reactions with carefully-considered responses during social interaction and the ability to be cognitively flexible enough to switch from one task to another10. It also plays key roles in your ability to maintain a goal-oriented mindset. Since some of the most common symptoms of depression include lack of motivation and an inability to maintain a controlled and flexible mindset, the dorsolateral prefrontal cortex is a natural choice as a target for TMS intended to treat depression.
When TMS was initially being tested as a treatment for depression, scientists and doctors raised questions regarding whether altering activity in the dorsolateral prefrontal cortex would impact patient’s cognitive abilities- after all, it would make sense that altering brain activity would influence patients’ ability to perform thought-intensive tasks. Several subsequent studies collectively suggested that people with depression who received TMS actually exhibit improved cognitive abilities7, including enhanced abilities for switching between tasks, as well as exhibiting controlled rather than impulsive behavior. This is good news for the future of TMS as a treatment for depression, but also complicates our understanding of why TMS is an effective treatment for this mental illness. Prior to these studies, it was assumed that TMS directly decreased depressive symptoms. However, it has also been shown that improvement in these specific cognitive abilities is linked to fewer depressive symptoms regardless of whether the cognitive changes are brought on by TMS. This creates a chicken-or-egg scenario in that it is unclear whether TMS is improving depressive symptoms which then heightens cognitive ability or vice versa, which means that future research is necessary to fully understand the precise mechanism by which TMS helps alleviate depressive symptoms. Regardless, the fact that directly altering brain activity can alleviate symptoms of depression supports the concept that depression could be the result of atypical brain activity leading to deficits in a person’s ability to embrace goal-oriented motivation and maintain a flexible and controlled mode of thought. As our understanding of the mechanism by which TMS works continues to develop, the hope is that we will also gain a stronger understanding of what causes depression.
TMS as a treatment for OCD
Given its success in alleviating symptoms of depression, TMS has also been tested as an intervention for other mental health disorders, one of which is obsessive-compulsive disorder (also known as OCD). People with OCD experience hard-to-control repetitive thoughts and behaviors that can majorly interfere with everyday life. In 2018, almost exactly a decade after being approved to use as a tool for treating depression, TMS was also approved for use in the treatment of OCD9.
While several brain areas have been tested as targets for TMS-mediated treatment for OCD, one of the most common is the medial prefrontal cortex. Much like the dorsolateral prefrontal cortex, the medial prefrontal cortex also plays a key role in cognitive and emotional functions and connects to a number of other brain areas7. Although we don’t fully understand what distinguishes the function of these two brain regions from each other, recent findings suggest that the medial prefrontal cortex is heavily involved in our ability to extinguish intense emotions like anxiety, whereas the dorsolateral prefrontal cortex more heavily mediates how enjoyable we perceive our own emotional experiences to be11. Patients who received TMS stimulation to medial prefrontal cortex experienced improvements in obsessive-compulsive symptoms that coincided with an improvement in attentiveness and the ability to recognize and correct errors. Much like in the context of depression, this supports the presence of abnormal brain activity that could make certain people prone to developing OCD. Also like we observe in the context of depression, it is unclear whether TMS causes an improvement in cognitive abilities that then helps improve symptoms, or directly improves symptoms which leads to betterment of the cognitive abilities in question. Clarifying this point with further research could improve our understanding of the underlying cause of OCD and provide exciting avenues to enhance our ability to develop more versatile treatments for OCD.
The future of TMS and what it tells us about mental illness
Largely due to its success as a treatment for depression, TMS is also being investigated as a potential treatment for a variety of other disorders related to the brain, including schizophrenia and Alzheimer’s disease. TMS is also not the only kind of neuromodulation– another method of directly altering brain activity called deep brain stimulation is commonly used in patients with a neurological disease called Parkinson’s disease. Importantly, this supports the concept that mental illness could be the result of a physical, underlying issue with how the brain is wired, and should not be attributed to character flaws as it was for so many years. With further study, the hope is that TMS will both become even more effective for treating mental health disorders.
References
1. Mental Illness – National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/statistics/mental-illness.
2. Cuijpers, P. et al. The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta-analysis of direct comparisons. World Psychiatry 12, 137–148 (2013).
3. Levy, K. N., Ehrenthal, J. C., Yeomans, F. E. & Caligor, E. The Efficacy of Psychotherapy: Focus on Psychodynamic Psychotherapy as an Example. Psychodyn. Psychiatry 42, 377–421 (2014).
4. Arroll, B. et al. Efficacy and Tolerability of Tricyclic Antidepressants and SSRIs Compared With Placebo for Treatment of Depression in Primary Care: A Meta-Analysis. Ann. Fam. Med. 3, 449–456 (2005).
5. Klomjai, W., Katz, R. & Lackmy-Vallée, A. Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS). Ann. Phys. Rehabil. Med. 58, 208–213 (2015).
6. van Rooij, S. J. H., Arulpragasam, A. R., McDonald, W. M. & Philip, N. S. Accelerated TMS – moving quickly into the future of depression treatment. Neuropsychopharmacology 49, 128–137 (2024).
7. Cognitive effects of focal neuromodulation in neurological and psychiatric disorders | Nature Reviews Psychology. https://www.nature.com/articles/s44159-024-00291-3.
8. Purves, D. et al. Long-Term Synaptic Potentiation. in Neuroscience. 2nd edition (Sinauer Associates, 2001).
9. Commissioner, O. of the. FDA permits marketing of transcranial magnetic stimulation for treatment of obsessive compulsive disorder. FDA https://www.fda.gov/news-events/press-announcements/fda-permits-marketing-transcranial-magnetic-stimulation-treatment-obsessive-compulsive-disorder (2024).
10. Dorsolateral Prefrontal Cortex – an overview | ScienceDirect Topics. https://www.sciencedirect.com/topics/neuroscience/dorsolateral-prefrontal-cortex.
11. Nejati, V., Majdi, R., Salehinejad, M. A. & Nitsche, M. A. The role of dorsolateral and ventromedial prefrontal cortex in the processing of emotional dimensions. Sci. Rep. 11, 1971 (2021).
Thumbnail photo was AI-generated using canva.com.
Figure 1 created in BioRender. Riley, J. (2024) https://BioRender.com/w51s827. Publication license agreement number IJ27KCNOG4.

Leave a comment