November 28th, 2022
Written by: Marissa Maroni
In the news or on your favorite medical drama you may have been startled to see patients are kept awake during brain surgery. If not, we’ve included an example here! Although it feels wild to witness awake surgeries, they’re possible because the brain itself cannot sense any pain. Despite the lack of pain sensed by the brain, most people do experience head pain at some point in their life, including headaches. The deep, throbbing pain, and sometimes nausea, experienced during a headache can be unbearable. But if brains can’t feel, what causes the pain of a headache and how is this treated?
What kinds of headaches are there?
There are three main types of primary headaches, primary meaning the headache is the issue, rather than a symptom from an underlying condition. The three types of primary headaches are:
1. Tension-type headaches
Tension-type headaches are the most common primary headache and impact over 25% of people globally1. Tension-type headaches are characterized by mild to moderate head pain that feels like a tightening pressure (imagine hands gripped tightly around your head) that affects both sides of the brain, lasting minutes up to several days2.
2. Migraines
Migraines effect approximately 14% of the global population1. Migraines are characterized as moderate to severe throbbing pain usually on one side of the brain with pain lasting from several hours to 3 days3. Migraines are usually accompanied by various symptoms such as nausea and light and sound sensitivity4.
3. Cluster Headaches
Cluster headaches affect approximately 0.4% of people5. Cluster headaches are characterized by excruciating pain on one side of the brain usually surrounding the eye that lasts for minutes up to 3 hours5.
How do they start?
Each of the three primary types of headaches vary in their origin. Rather than extensively unpacking each, let’s focus in on migraines. Prior to a migraine starting a person can experience sound and light sensitivity, mood changes, thirst, and yawning among other symptoms. Scientists have used brain imaging prior to the start of migraines to try and understand why do they start in the first place and what could be causing pre-migraine symptoms?
It is theorized that the brainstem, the stalk of your brain that controls breathing and heart rate among other functions, is the generator of migraines6. A brain imaging study found activity in a subregion of the brainstem was associated with the time until the next migraine starts7. Further, a set of researchers from Germany imaged the brain of a migraine patient for 30 consecutive days to understand what events occur in the brain leading up to a migraine8. They found that before and during a migraine there is altered communication between the brainstem and the hypothalamus, a part of the brain important in controlling sleep, hunger, thirst, and more. Additionally, they found increasing activity in the hypothalamus in the time leading up to a migraine.
Scientists have identified critical brain regions that have altered brain activity prior to a migraine, but can any of this explain pre-migraine symptoms? Researchers hypothesize that the increased activity in the hypothalamus could explain pre-migraine symptoms such as yawning and thirst. Interestingly, migraine patients with light sensitivity have increased activation of the occipital cortex, a brain region responsible for vision perception, in comparison to migraine patients who did not experience light sensitivity9. Although the answer is not precise, scientists have identified altered brain signaling that may prime a brain for a migraine attack and identified specific brain regions that can explain pre-migraine symptoms.
Where does the pain come from?
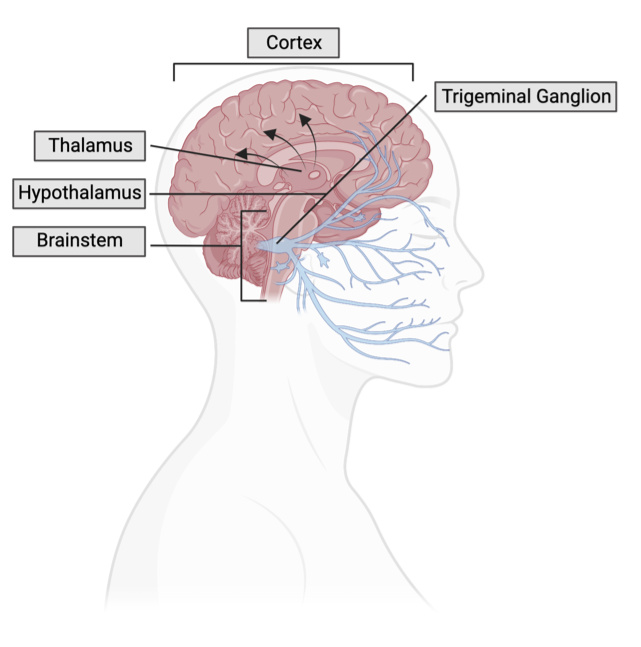
A main piece to the migraine pain puzzle is a group of nerves that carry pain signals from the face to the brain, referred to as trigeminal ganglion. The trigeminal ganglion connect to the blood vessels surrounding your brain and various parts of the brain including the brainstem, hypothalamus, and thalamus (Figure 1). The thalamus is a place for information to be relayed to your cortex. The activation of trigeminal ganglion lead to a cascade of events that have roles in migraine pain. Let’s explore what events occur and how they contribute to migraine pain.
Sensitization of the brain
During a migraine, it is thought that the trigeminal ganglion become sensitized, meaning they can activate and send pain signals in response to nonpainful stimuli (Figure 2)3. Trigeminal ganglion sensitivity causes throbbing head pain, and pain felt when coughing or bending over during a migraine. Even though you are not doing anything to cause this pain, the trigeminal ganglion is sensitized and sending pain signals anyway! The sensitized trigeminal ganglion lead to the activation and sensitization of the brainstem, and thalamus10. Sensitization of the brainstem and thalamus contribute to allodynia, perception of pain by something not normally painful, like a gentle touch or glasses resting on your nose. Collectively, the sensitization of the trigeminal ganglion, brainstem, and thalamus play a critical role in migraine pain.
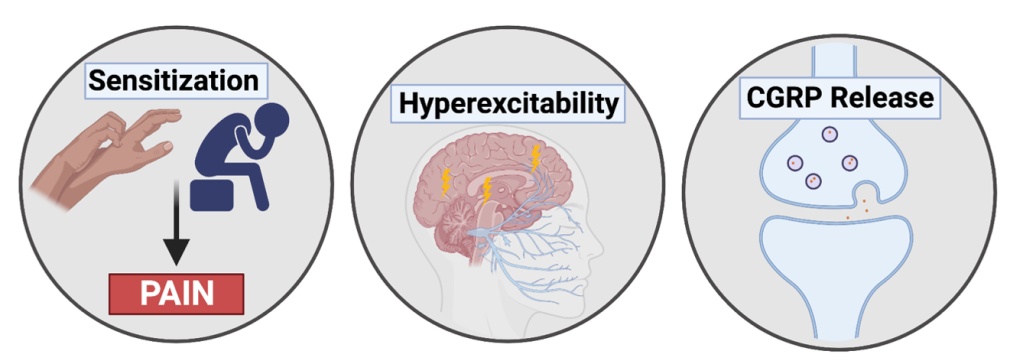
Figure 2. Three contributors to migraine pain: sensitization, hyperexcitability, and CGRP release.
Hyperexcitability
Hyperexcitability refers to neurons that are more likely to become active and send signals. General hyperexcitability is seen in individuals with migraines and is hypothesized to contribute to sensitization in the brain as there is more activation in pain signaling regions (Figure 2)3. Brain imaging studies identified that during a migraine the brain is hyper-responsive to sensory information3. This hyper-responsiveness is hypothesized to cause light sensitivity during migraines. Interestingly, when scientists examined shared mutations in the genes of migraine patients, they found that many of the mutated genes were important in neuronal signaling, further suggesting a role for hyperexcitability in migraines11.
Neuropeptide release
The activation of the trigeminal ganglion causes the release of neuropeptides. Neuropeptides are small proteins that cause changes in neuronal signaling (oxytocin is a well-known example of a neuropeptide). An important neuropeptide released after trigeminal ganglion activation is calcitonin-gene related peptide (CGRP). CGRP modulates pains signals, mediates inflammation in the brain, and has cardiovascular, functions among other roles 3,12. There is evidence that CGRP initiates and maintains the sensitization of trigeminal ganglion and is involved in signaling between trigeminal nerves3,13. Further, intravenous administration of CGRP triggers a migraine in migraine patients but not in healthy individuals, suggesting CGRP plays a key role in migraines10. Additionally, CGRP causes blood vessels surrounding the brain to dilate, meaning they expand however, the contribution of blood vessel expansion in migraine pain is disputed14.
What are some treatment for migraines?
Scientists have identified several changes in brain function before and during a migraine that contribute to migraine pain. With all this known, how are migraines treated and how do these treatments work?
A popular and effective treatment for migraines during an active attack are triptans. Triptans act on serotonin receptors. Serotonin is a chemical messenger within our brain responsible for a variety of functions, including mood and digestion. When triptans act on serotonin receptors, they inhibit pain neurotransmission in the trigeminal ganglion, inhibit the release of pain-promoting neuropeptides (like CGRP!), and constrict blood vessels15. Given what we know about headaches, this drug works by halting the cascade of events that occur during a migraine including sensitization, hyperexcitability, and neuropeptide release.
Overall, we’ve uncovered changes in brain signaling that occur before and during a migraine, along with a current treatment. Even though the brain itself cannot feel any pain, it plays a critical role in communicating pain to different parts of your body!
References
- Stovner, L. J., Hagen, K., Linde, M., & Steiner, T. J. (2022). The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. The journal of headache and pain, 23(1), 1-17.
- Ashina, S., Mitsikostas, D. D., Lee, M. J., Yamani, N., Wang, S. J., Messina, R., … & Lipton, R. B. (2021). Tension-type headache. Nature Reviews Disease Primers, 7(1), 1-21.
- Dodick, D. W. (2018). A phase‐by‐phase review of migraine pathophysiology. Headache: the journal of head and face pain, 58, 4-16.
- Pescador Ruschel MA, De Jesus O. Migraine Headache. 2022 Jul 6. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 32809622.
- Rossi, P., Whelan, J., Craven, A., & De La Torre, E. R. (2016). What is cluster headache? Fact sheet for patients and their families. A publication to mark Cluster Headache Day 2016. Functional Neurology, 31(3), 181.
- Puledda, F., Messina, R., & Goadsby, P. J. (2017). An update on migraine: current understanding and future directions. Journal of neurology, 264(9), 2031-2039.
- Stankewitz, A., Aderjan, D., Eippert, F., & May, A. (2011). Trigeminal nociceptive transmission in migraineurs predicts migraine attacks. Journal of Neuroscience, 31(6), 1937-1943.
- Schulte, L. H., & May, A. (2016). The migraine generator revisited: continuous scanning of the migraine cycle over 30 days and three spontaneous attacks. Brain, 139(7), 1987-1993.
- Karsan, N., & Goadsby, P. J. (2018). Biological insights from the premonitory symptoms of migraine. Nature Reviews Neurology, 14(12), 699-710.
- Pietrobon, D., & Moskowitz, M. A. (2013). Pathophysiology of migraine. Annual review of physiology, 75, 365-391.
- Burstein, R., Noseda, R., & Borsook, D. (2015). Migraine: multiple processes, complex pathophysiology. Journal of Neuroscience, 35(17), 6619-6629.
- Russo, A. F. (2015). Calcitonin gene-related peptide (CGRP): a new target for migraine. Annual review of pharmacology and toxicology, 55, 533.
- Iyengar, S., Johnson, K. W., Ossipov, M. H., & Aurora, S. K. (2019). CGRP and the trigeminal system in migraine. Headache: The Journal of Head and Face Pain, 59(5), 659-681.
- Buture, A., Gooriah, R., Nimeri, R., & Ahmed, F. (2016). Current understanding on pain mechanism in migraine and cluster headache. Anesthesiology and Pain Medicine, 6(3).
- Johnston, M. M., & Rapoport, A. M. (2010). Triptans for the management of migraine. Drugs, 70(12), 1505-1518.
Cover photo by Robin Higgins from Pixabay
Figures created with BioRender.com.

Leave a comment