October 1st, 2024
Written by: Lindsay Ejoh
Have you or a loved one ever been doubled over in pain during a period? Pain is a common menstrual symptom, but some people experience debilitating period pain– the kind that lasts for hours to days, prevents you from living out your daily life, and does not let up with painkillers. They may also feel extreme fatigue, pain during urination, or even have severe gastrointestinal issues around the time of their period These symptoms could be more than just bad period cramps– it could be a sign of an underlying condition called endometriosis1. Let’s unpack what causes this painful condition, the existing treatment options, and what questions scientists still need to answer to build more effective avenues for treatment.
What is endometriosis?
First, it’s important to understand that though endometriosis affects approximately 1 in 10 people with uteruses2, not everyone with severe period pain has endometriosis. To understand this specific condition, we must break down the anatomy of the typical female human reproductive system (Figure 1). The uterus (Figure 1E) stores eggs in its walls, or lining, called the endometrium (Fig 1C). Every month (typically), these eggs either get fertilized by sperm, or shed and exit the body through menstrual blood.
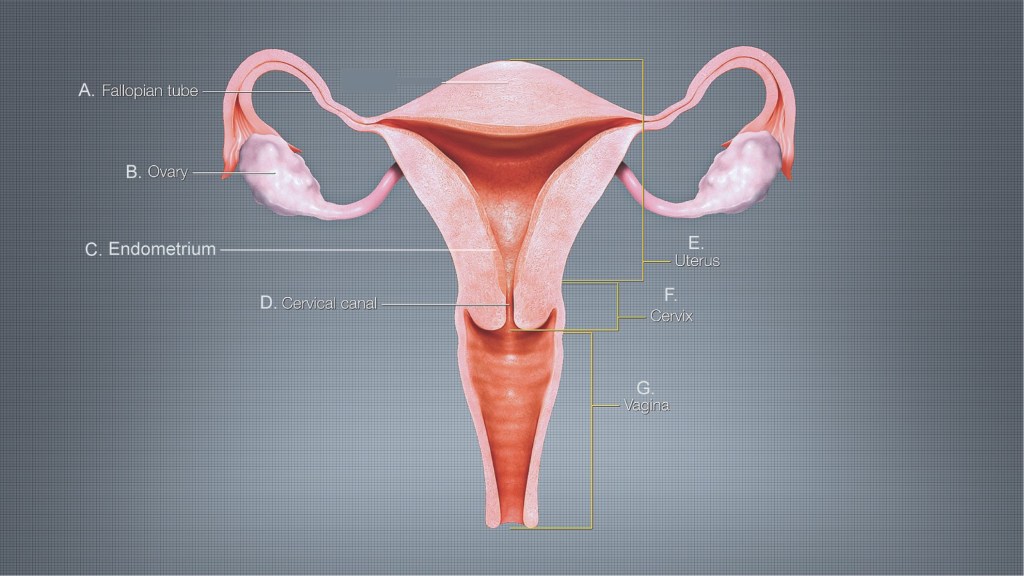
Endometriosis is defined by endometrial-like tissue (which resembles the endometrium, but is not exactly the same) growing outside the walls of the uterus- on the ovaries, bladder, intestines, appendix, or even in the abdominal cavity, where it doesn’t belong3. Despite growing in the wrong places, the tissue can still act like endometrium— thickening, breaking down, and shedding during the menstrual cycle4,5. Unlike menstrual blood that passes through the cervical canal (Figure 1D), this blood pools up in the abdominal cavity with nowhere to go, leading to inflammation, fertility issues, and pelvic pain.
Origins of endometriosis
The exact cause of endometriosis is unknown, but the prevailing theory is that menstrual blood moves backwards, a phenomenon called retrograde menstruation6. During retrograde menstruation, the menstrual blood made of the shed endometrial lining moves up through the fallopian tubes (Figure 1A) and spills out into the abdominal cavity, rather than going down through the cervical canal (Figure 1D) and out the vagina (Figure 1G). Blood that moves backwards and into the fallopian tubes is able to leak out into the surrounding abdominal cavity because the fallopian tubes are not completely closed off at their end closest to the ovaries (Figure 1B). Retrograde menstruation could explain how endometrial-like tissue starts growing outside of the uterus in the first place. However, this does not fully explain the cause of endometriosis, since most people who menstruate experience retrograde menstruation, but most people do not develop endometriosis. Scientists are also exploring how hormonal and immunological factors cause endometriosis5.
Endometriosis pain
Though other symptoms occur with endometriosis, abdominal pain can be the most debilitating. Misplaced endometrial-like tissue in the abdominal cavity triggers activation of the immune system6, your body’s defensive line that recognizes that the endometrial-like tissue is not supposed to be there. As a result, the immune system mounts an attack called inflammation, working to “fight off” the foreign cells and begin the healing process. Despite efforts from immune cells, the rogue endometrial-like tissue still remains, sticking to the abdominal cavity walls or surrounding organs and recruiting their own supply of blood, as well as nerves to sense the area. These nerves sense the inflammation in the area and send pain signals to the brain.
The exact mechanisms of endometriosis pain are still a mystery to scientists. Oddly enough, the pain experienced during endometriosis varies widely between patients, and isn’t explained by the amount, size, or types of misplaced endometrial tissue. Interestingly, 30% of patients with endometriosis experience pain that is unresponsive to any medication or surgery7. Scientists think these patients have undergone changes in their brain and spinal cord chemistry that lead to increased sensitivity to pain6. Pain that can’t be explained by a specific bodily injury occurs with other chronic pain disorders too, like fibromyalgia, inflammatory bowel disorder, and some types of migraine disorders.
Getting diagnosed with endometriosis
Unfortunately, as of now, the only way to get an official endometriosis diagnosis is through surgical intervention5. A gynecologist must cut into the abdomen and cut out samples of tissue and submit them to a lab for testing to confirm the presence of endometrial-like tissue outside the uterus. This often delays diagnosis– on average, it takes 7-10 years from the onset of symptoms for someone to get a proper diagnosis2. 60% of patients see 3+ clinicians before receiving a diagnosis8. Unfortunately, many people with endometriosis have to fight to get this painful condition taken seriously by doctors, further delaying the care they need.
Treating endometriosis
Currently, there is no cure for endometriosis pain. Treatment options for endometriosis include hormone supplements and other medications, surgery, and non-medical interventions6. Taking hormonal birth control, which works to suppress estrogen in the body and slow the growth of the misplaced endometrial tissue, is currently the most effective treatment for endometriosis. However, symptoms return if the patient stops taking them, which is not suitable for people who want to be pregnant. Non-steroidal anti-inflammatory drugs, like Ibuprofen, can help curb pain too, but are not suitable for long-term use due to harmful side effects.
Surgery to remove the misplaced tissue also helps, but is not a perfect option. Since endometrial-like tissue can grow on multiple different organs in the abdomen, it can be difficult for surgeons to remove it all. As a result, 21.5% of patients experience a relapse in pain again after two years, and 40-50% relapse 5 years after surgery9.
Though we do not have a cure, there are non-drug interventions like pelvic physical therapy and cognitive behavioral therapy that can be especially helpful for the 30% of patients that aren’t helped by existing medications or surgeries 6. Endometriosis can affect everyone differently and impacts multiple bodily systems. Therefore, treatment plans should be personalized and treat the whole body to ensure the best outcomes for patients.
A critical need for more research
In 2022, the National Institutes of Health (a government agency that funds most of the biomedical research in the United States) dedicated $16 million to endometriosis research10. While this might seem like there are quite a lot of tax dollars going to this issue, it’s miniscule compared to the $90 million spent on Crohn’s disease, $2.6 billion on heart disease, and $7.6 billion on cancer research that year11. Though many people are affected by endometriosis, funding is limited, and there is a desperate need for more research to understand the exact causes of the condition and the chronic pelvic pain it causes, so we improve our limited diagnosis and treatment options.
If you or someone you know who menstruates struggles with long and painful periods, fertility issues, pain during sex, bowel issues, and chronic fatigue, it’s worth talking to a clinician about the possibility of endometriosis. Don’t be afraid to get a second opinion if your concerns aren’t taken seriously. While it can be exhausting to fight for your health, getting the right diagnosis can be life-changing. For those battling endometriosis, your strength is inspiring. Scientists and doctors and loved ones, be encouraged to spread awareness about this debilitating yet massively understudied condition so that we can get more resources, more research, and ultimately, more effective and accessible treatments for everyone with endometriosis!
References
- Wisely, R. (2022, November 11). Endometriosis: 9 facts to know about the puzzling disease. Michigan Medicine. https://www.michiganmedicine.org/health-lab/endometriosis-9-facts-know-about-puzzling-disease
- Endometriosis facts and figures. Endometriosis UK. (n.d.). https://www.endometriosis-uk.org/endometriosis-facts-and-figures
- Horne, A. W., & Missmer, S. A. (2022). Pathophysiology, diagnosis, and management of endometriosis. BMJ (Clinical research ed.), 379, e070750. https://doi.org/10.1136/bmj-2022-070750
- Shirazi, N., Nautiyal, R., & Jindal, R. (2023). Clinical pattern and spectrum of atypical endometriosis: A series of 5 cases. International Journal of Innovative Research in Medical Science, 8(03), 129–132. https://doi.org/10.23958/ijirms/vol08-i03/1645
- Mayo Foundation for Medical Education and Research. (2024, August 30). Endometriosis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656#:~:text=With%20endometriosis%2C%20bits%20of%20the,tissue%20does%20during%20menstrual%20cycles.
- Saunders, P. T. K., & Horne, A. W. (2021). Endometriosis: Etiology, pathobiology, and therapeutic prospects. Cell, 184(11), 2807–2824. https://doi.org/10.1016/j.cell.2021.04.041
- Coccia, M. E., Rizzello, F., Palagiano, A., & Scarselli, G. (2011). Long-term follow-up after laparoscopic treatment for endometriosis: multivariate analysis of predictive factors for recurrence of endometriotic lesions and pain. European journal of obstetrics, gynecology, and reproductive biology, 157(1), 78–83. https://doi.org/10.1016/j.ejogrb.2011.02.008
- Greene, R., Stratton, P., Cleary, S. D., Ballweg, M. L., & Sinaii, N. (2009). Diagnostic experience among 4,334 women reporting surgically diagnosed endometriosis. Fertility and sterility, 91(1), 32–39. https://doi.org/10.1016/j.fertnstert.2007.11.020
- Guo S. W. (2009). Recurrence of endometriosis and its control. Human reproduction update, 15(4), 441–461. https://doi.org/10.1093/humupd/dmp007
- Giudice, L. C., Horne, A. W., & Missmer, S. A. (2023). Time for global health policy and research leaders to prioritize endometriosis. Nature communications, 14(1), 8028. https://doi.org/10.1038/s41467-023-43913-9
- NIH funding for cancer: https://www.statista.com/statistics/716597/total-cancer-funding-by-the-national-institutes-for-health/
Figure 1 modified from Wikimedia Commons
Cover photo from blauthbianca on Pixabay

Leave a comment